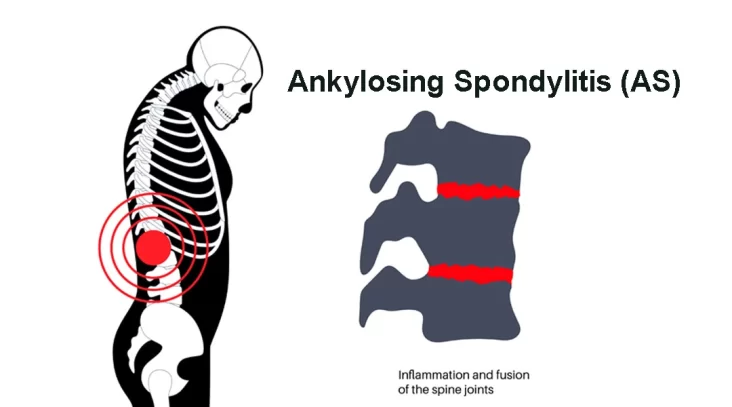
Ankylosing spondylitis (AS) is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints, characterized by pain, stiffness, and eventual fusion of the vertebrae. This condition falls under the category of spondyloarthritis, a group of rheumatic diseases that share similar features.
Symptoms and Progression
The hallmark symptom of Ankylosing spondylitis (AS) is back pain and stiffness, typically worse in the morning or after periods of inactivity. This stiffness often improves with movement and exercise. Over time, the inflammation can lead to the formation of new bone, causing the vertebrae to fuse together, resulting in a loss of mobility and flexibility in the spine. AS can also affect other joints such as the hips, shoulders, and knees, as well as other organs like the eyes, heart, and lungs.
Causes: The exact cause of Ankylosing spondylitis (AS) is unknown, but it is believed to involve a combination of genetic and environmental factors. The majority of individuals with AS carry the HLA-B27 gene, although not everyone with this gene develops the condition. Environmental factors such as bacterial infections may trigger the immune system to attack the body’s own tissues, leading to inflammation and damage.
Diagnosis: Diagnosing AS can be challenging, as its symptoms can overlap with other conditions like mechanical back pain or other types of arthritis. A comprehensive evaluation by a rheumatologist typically includes a medical history, physical examination, blood tests to check for inflammation and the presence of the HLA-B27 gene, and imaging studies such as X-rays or MRI scans to assess for structural changes in the spine and joints.
Treatment: The goals of treatment for Ankylosing spondylitis (AS) are to relieve pain, reduce inflammation, preserve mobility, and prevent complications. This often involves a combination of medications, physical therapy, and lifestyle modifications. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to alleviate pain and inflammation. Disease-modifying antirheumatic drugs (DMARDs) and biologic agents may be prescribed to suppress the underlying inflammatory process. Physical therapy and regular exercise are essential for maintaining flexibility and strength in the spine and joints. In severe cases where joint damage is extensive, surgery may be necessary to correct deformities or replace damaged joints.
Prognosis: AS is a chronic condition that tends to progress slowly over time. While there is currently no cure, early diagnosis and appropriate management can help control symptoms and delay or prevent complications. With proper treatment, many individuals with AS are able to lead active and productive lives. However, some may experience significant disability and impairment in quality of life, particularly if the disease is not adequately controlled.
Living with AS: Living with AS can be challenging both physically and emotionally. Chronic pain and stiffness can impact daily activities and social interactions, leading to feelings of frustration, isolation, and depression. Building a support network of healthcare professionals, family, and friends can provide valuable encouragement and assistance. Learning coping strategies, managing stress, and maintaining a healthy lifestyle are important aspects of self-care for individuals with AS.
Ankylosing spondylitis (AS) is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints. It is characterized by pain, stiffness, and eventual fusion of the vertebrae, leading to loss of mobility and flexibility. Early diagnosis and appropriate management are crucial for controlling symptoms and preventing complications. While there is currently no cure, with proper treatment and self-care, many individuals with AS can lead fulfilling lives. Ongoing research into the underlying mechanisms of the disease and the development of new treatment approaches offer hope for improved outcomes in the future.